Testicular Mesothelioma
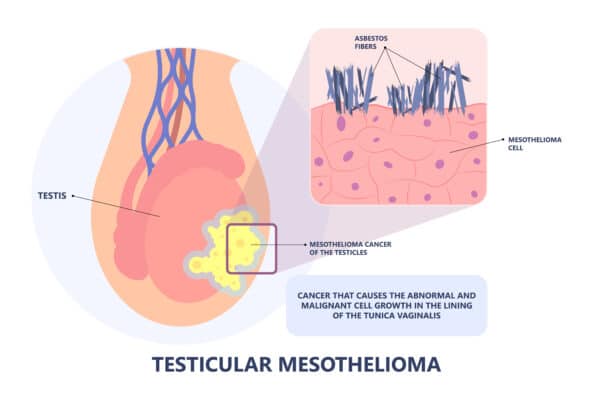
Testicular mesothelioma is a rare form of malignant mesothelioma that affects the lining of the testicles. This form of cancer is closely linked to exposure to asbestos, a mineral once widely used in various industries.
It originates in the tunica vaginalis membrane that envelops the testis. The median age at diagnosis of testicular mesothelioma is approximately 60 years. Due to its extreme rarity, limited research exists, and there are no established standard treatments specifically for this form of cancer. However, treatment approaches used for other types of mesothelioma have shown some effectiveness.
Survival & Prognosis for Testicular Mesothelioma
Several factors influence the prognosis of testicular mesothelioma, including the stage at which it is diagnosed, the chosen treatment method, and the overall health of the patient. With appropriate treatment, the average survival rate for testicular mesothelioma is around five years. This is a relatively favorable prognosis compared to other types of mesothelioma.
Survival Statistics for Testicular Mesothelioma:
- Median Survival: Approximately five years
- 5-Year Survival Rate: 58%
- 10-Year Survival Rate: 45%
Recent studies have indicated an improvement in survival rates, with some cases achieving a median survival of over five years. This improvement can be attributed to surgical interventions, regular monitoring for recurrence, and advancements in treatment options.
Symptoms of Testicular Mesothelioma
Testicular mesothelioma typically presents with painless symptoms, commonly involving swelling of the scrotum. Hydrocele, the accumulation of fluid around the testicle, is a frequent symptom experienced by more than half of patients. Notably, several other medical conditions can produce symptoms similar to those of testicular mesothelioma, making an accurate diagnosis challenging.
Common Symptoms of Testicular Mesothelioma:
- Enlargement of the scrotum (scrotal swelling)
- Hydrocele (abnormal fluid retention around the testicle)
- Inguinal mass (resembling an inguinal hernia)
- Solid scrotal mass (paratesticular mass)
- Spermatocele (a fluid-filled area in the spermatic cord)
Given the non-specific nature of these symptoms, individuals who suspect they may have testicular mesothelioma, especially those with a history of asbestos exposure, should consult a healthcare professional for a thorough evaluation.
Diagnosing Testicular Mesothelioma
Diagnosing testicular mesothelioma involves a series of steps, which may include surgical removal and examination of potential tumor tissue. Physicians typically order various diagnostic tests to confirm the presence of testicular mesothelioma. These tests may encompass CT scans, immunohistochemistry testing, tissue biopsies, and ultrasound imaging.
Due to the rarity of testicular mesothelioma and its non-specific symptoms, arriving at an accurate diagnosis can be challenging. In some cases, patients are only diagnosed after undergoing surgery, and immunohistochemistry testing is often necessary to establish a definitive diagnosis.
Evaluating the Stages of Testicular Mesothelioma
Medical professionals use staging to assess the extent of cancer spread in testicular mesothelioma. Staging aids in determining the most suitable treatment approach. TNM is a system, adapted for testicular cancer, and is employed for staging, considering factors like the size and extent of the tumor (T), involvement of nearby lymph nodes (N), and distant cancer spread (M).
Early diagnosis of testicular mesothelioma is relatively common, with more than half of cases detected at or before the T2 stage. Earlier stages generally present a more favorable prognosis, though it’s important to note that staging does not solely dictate prognosis. Nevertheless, staging can guide treatment decisions and potentially offer more treatment options.
Exploring Treatment Options
Treatment for testicular mesothelioma is not yet standardized due to its extreme rarity. However, surgery, particularly radical orchiectomy, is frequently employed and has demonstrated effectiveness. In some cases, additional treatments such as chemotherapy, immunotherapy, and radiation may be recommended by healthcare professionals.
Radical orchiectomy, involving the removal of the affected testicle and spermatic cord, is a common surgical procedure used in treating testicular mesothelioma. It is often followed by the option of a testicular prosthesis for cosmetic purposes.
While case reports mention non-surgical treatments, such as radiation therapy and chemotherapy, there is limited data available regarding their impact on long-term survival. Nonetheless, testicular mesothelioma survival rates remain relatively favorable, and palliative care can help patients manage treatment side effects and maintain their quality of life.
Testicular Mesothelioma Causes
Researchers studying testicular mesothelioma and its causes face unique challenges. While some cases have been associated with asbestos exposure, the precise mechanism by which asbestos fibers lead to the development of testicular mesothelioma remains unclear.
Asbestos fibers may reach the tunica vaginalis membrane surrounding the testis, potentially triggering inflammation and genetic damage within cells, which could contribute to cancer development. However, further research is needed to fully elucidate the exact pathophysiology.
It is crucial to recognize that testicular mesothelioma is exceptionally rare, and most individuals exposed to asbestos do not develop this specific form of cancer. Asbestos exposure remains a known risk factor, but the mechanisms involved are complex and necessitate ongoing scientific investigation.
In conclusion, testicular mesothelioma is a rare and challenging form of cancer linked to asbestos exposure. While progress has been made in understanding and treating this condition, ongoing research is crucial to improve diagnosis and treatment outcomes. Patients and healthcare providers should remain vigilant, especially in cases of suspected asbestos exposure, and consult experts in the field for guidance and care.
