Pleurodesis Surgery for Mesothelioma
Pleurodesis is a medical procedure aimed at addressing and preventing pleural effusions, a common complication associated with malignant pleural mesothelioma. While it does not offer a cure for this aggressive cancer, pleurodesis plays a crucial role in relieving distressing symptoms, especially difficulty breathing.
What is Pleurodesis?
Pleurodesis serves as both a treatment and a preventive measure for pleural effusions. These effusions often manifest as dry coughs, chest pain, and, most notably, difficulty breathing. The primary objective of pleurodesis is to collapse the pleural space, thus preventing the buildup of excess fluid and alleviating these debilitating symptoms.
Pleural Effusions
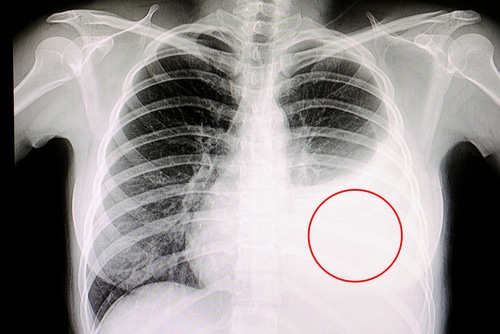
In a healthy state, the human lung is enveloped by a small amount of watery fluid, typically measuring just a few teaspoons. This fluid aids in the lung’s normal functioning. However, when an abnormal accumulation of fluid occurs within the pleural cavity— the space between the lung’s two surrounding membranes— a pleural effusion is diagnosed.
While various conditions can trigger pleural effusions, they are an especially prevalent symptom in individuals with pleural mesothelioma. In fact, an overwhelming majority, ranging from 80% to 95%, of pleural mesothelioma patients experience pleural effusions.
The Role of Pleurodesis in Managing Mesothelioma Symptoms
Pleurodesis is a crucial procedure for mesothelioma patients grappling with pleural effusions. It’s important to note that pleurodesis doesn’t offer a cure for mesothelioma; instead, it serves as a palliative treatment. By addressing the symptoms stemming from fluid buildup, pleurodesis enhances a patient’s overall quality of life.
Patients afflicted with pleural mesothelioma and accompanying pleural effusions often contend with debilitating issues such as breathlessness, chest pain, and persistent dry cough. Pleurodesis steps in to provide much-needed relief by effectively draining and preventing the recurrence of excess fluid.
Comparing Pleurodesis and Thoracentesis
The choice between pleurodesis and thoracentesis (also known as pleurocentesis) hinges on an individual’s unique case and circumstances.
- Thoracentesis (Pleurocentesis): This procedure involves the drainage of excess fluid from the pleural space using a needle. It may need to be repeated multiple times to provide symptom relief.
- Pleurodesis: Pleurodesis offers a more lasting solution by preventing the reaccumulation of fluid in certain cases. It is considered a long-term strategy to manage pleural effusions.
The Types of Pleurodesis
Pleurodesis can be carried out through two distinct methods: chemical pleurodesis and mechanical pleurodesis. Each approach has its own set of advantages and risks, and the choice between them is determined by the patient’s medical team based on their specific situation.
- Chemical Pleurodesis: This method involves the introduction of a chemical substance into the pleural cavity, often medical-grade talc or doxycycline, via a chest tube. The substance induces inflammation and scarring, leading to the adherence of pleural layers and the reduction of fluid buildup. This procedure typically requires several hours and is performed under anesthesia. Patients may need to stay in the hospital for five to seven days following chemical pleurodesis.
- Mechanical Pleurodesis: Unlike chemical pleurodesis, this method relies on mechanical intervention. Surgeons induce inflammation and scarring by mechanically causing abrasions (scratches) on the pleural membranes. This scarring prevents further fluid accumulation, offering relief to patients.
Recovery Following Pleurodesis
The recovery period following pleurodesis can vary depending on several factors, including the patient’s overall health and the specific type of pleurodesis procedure performed (chemical, mechanical, or rapid).
In most cases, hospitalization is necessary until the chest tubes can be safely removed. This typically occurs within about five to seven days for patients who undergo chemical or mechanical pleurodesis. Rapid pleurodesis may result in a shorter hospital stay.
After the chest tubes are removed, it’s common for the wound to continue draining for one to two days. During this time, patients are advised to leave the bandage in place. It’s important to keep the incision area clean and dry, avoiding the application of creams, ointments, or powders. Submerging the wound in water should also be avoided until it has fully healed.
Patients should follow the guidance of their healthcare team regarding when it’s safe to return to their normal activities. It’s essential to report any side effects or concerns to the healthcare professionals overseeing their care.
Benefits and Considerations
Pleurodesis focuses on easing the symptoms linked with malignant pleural effusions. These symptoms may include:
- Dry cough
- Chest tightness
- Difficulty breathing
- Chest pain
- Discomfort when not in an upright position
By addressing these distressing symptoms, pleurodesis can significantly enhance a patient’s quality of life. In fact, According to the National Library of Medicine, research has suggested that pleurodesis may extend the life expectancy of pleural mesothelioma patients. For those who undergo pleurodesis alone, the median survival was reported to be 12 months, compared to just six months for untreated pleural mesothelioma patients.
Evaluating Risks and Complications
As with any medical procedure, pleurodesis carries inherent risks, which can vary based on the patient’s individual case and the type of pleurodesis performed. Common risks and side effects may include:
- Chest pain or tightness
- Fever
- Infection, which may necessitate antibiotic treatment
In rare cases, more severe complications such as acute respiratory distress syndrome (ARDS) or heart issues may arise post-pleurodesis. ARDS, characterized by fluid accumulation in the lung’s air sacs, can lead to serious breathing difficulties.
Patients must weigh the potential benefits of pleurodesis against these risks, with the guidance of their healthcare team. While patients with stage 4 mesothelioma may not be suitable candidates for pleurodesis, those in earlier stages and good health can explore this option as part of their treatment plan.
Ultimately, patients are encouraged to engage in open discussions with their healthcare providers to fully understand their treatment options, including the associated risks and benefits.
